One of the largest gene-based collapsing analyses reveals potential candidate genes for population screening

Short on time? Watch this short, two-minute video wherein Helix Scientist Elizabeth Cirulli, Ph.D., walks you through the paper and its findings.
Over the last decade, several population genomic screening programs have been launched in an effort to improve healthcare through DNA sequencing. Evidence suggests that many people in the general public have inherited genetic factors that greatly increase their risk for disease that, if detected early, could be managed.
However, the majority of these at-risk individuals have yet to develop symptoms and may not have any overt red flags in their family’s medical history, meaning it is very unlikely that they’ll become aware of their increased disease risk, much less take action to manage it. This is where large-scale genetic screening initiatives—like those offered through population genomics projects—can make a big difference.
Projects like Renown Health’s Healthy Nevada Project or Mayo Clinic’s Tapestry accept all comers with very few limitations, meaning apparently healthy individuals gain access to genetic screening. Historically, such testing was only available to individuals with symptoms of disease or a suspect family history of disease.

The scope of genetic screening is often focused on select, highly impactful conditions—primarily Familial Hypercholesterolemia (FH), Hereditary Breast and Ovarian Cancer (HBOC), and Lynch syndrome (LS), collectively known as the CDC Tier 1 (CDCT1) conditions. Importantly, genetic variants related to these conditions are highly penetrant, significantly increase the odds of disease development over non-carriers, and medical guidelines exist to help manage the disease at an early stage.
Evidence thus far suggests that as much as 1:75 individuals carry a variant for one of these conditions, and that 90% of carriers were unaware prior to participating in a population genomics project.
While the inclusion of the CDCT1 conditions in screening programs is highly beneficial, there may be room to expand the impact of screening programs by including additional genetic conditions. A recent paper from the Helix research team, published in Genetics In Medicine, presents evidence that four additional gene-disease associations warrant consideration: GCK with diabetes mellitus, HBB with hemoglobinopathies, PKD1 with cystic kidney disease, and MIP with cataracts.
One of the largest gene-based collapsing analyses on rare variants
Helix’s research team analyzed both genetic and medical records data from >220,000 individuals in two large cohorts—the Healthy Nevada Project and the UK Biobank—in a gene-based collapsing analysis using rare variants. The scale of this analysis makes it one of the largest in the field and gave researchers a powerful opportunity to identify significant gene-disease associations.
Analyses revealed 74 significant gene-disease associations across 27 genes. Among these, seven of the associations had positive predictive values (PPVs) that were ≥ 30%. PPV, also known as penetrance, is an indication of how likely it is that a variant will lead to a disease. Notably, CDCT1 conditions have reported PPV values within the same range as these seven conditions.
Three of the conditions overlapped with CDCT1 conditions, specifically HBOC and FH and represented 79% of carriers within the two cohorts. The remaining 21% of carriers, however, had variants related to one of four gene-disease associations: GCK with diabetes mellitus, HBB with hemoglobinopathies, PKD1 with cystic kidney disease, and MIP with cataracts.
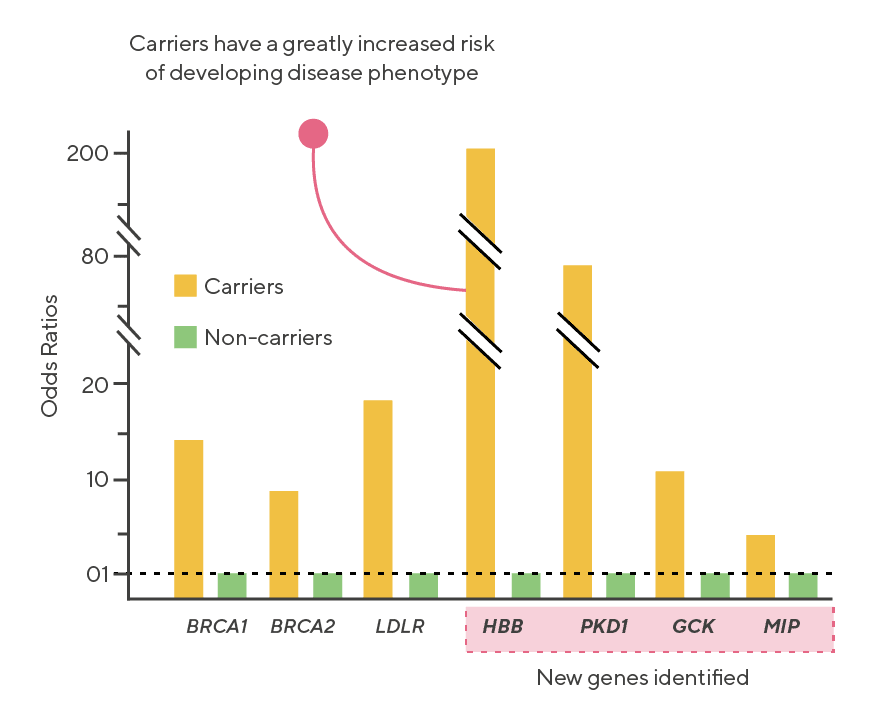
These four conditions all showed high PPV values (ranging from 43-59% in some populations) and odds ratios as high as 197 (HBB with hemoglobinopathies), indicating an almost 200 fold increase in risk of condition development among carriers relative to non-carriers.
Given their high penetrance and odds ratios, these four gene-disease associations warrant consideration for inclusion in population genomics and other large-screening initiatives. According to this study, including these four gene-disease associations may increase detection of at risk individuals by as much as 27%.
Put simply, large-genetic screening programs have the power to improve healthcare outcomes for many, and the potential for including these four additional gene-disease associations warrants consideration when planning such projects.