The enduring nature of COVID-19

Symptoms of COVID-19 may endure for months after infection, even in people who initially experienced mild illness. This is the conclusion put forth by a collaborative team of researchers from Helix, Renown Health, and the Desert Research Institute after analyzing survey data from more than 21,000 individuals, 233 of which report having tested positive for COVID-19.
We’re also presenting this work at the American Society of Human Genetics conference (#ASHG20). Click here to see our poster on this work.
Background
As the nation roiled in the wake of the COVID-19 pandemic, Helix researchers saw an opportunity to help. Over the past several years, Helix has cultivated a large community of people who are interested in helping advance science through genetic research. This community includes tens of thousands of individuals from Nevada who had entered the Helix community via the Healthy Nevada Project—a large population genomics study being run by Renown Health and the Desert Research Institute. Researchers realized early in the pandemic that genetic factors may help explain why some people experience severe symptoms of COVID-19 while others do not.
Helix’s research community is well suited to help answer this question because they have already contributed genetic data through Helix’s Exome+® assay and, unlike many other studies, represent a broad spectrum of demographics—consisting of people from many different cultures, socioeconomic backgrounds, and varying exposure to the SARS-CoV-2 (the virus responsible for COVID-19).
Researchers at both Helix and the Healthy Nevada Project sent out surveys asking individuals a series of questions regarding their exposure to the virus, whether they had been tested, what the test results were, if they had been experiencing any symptoms, and for how long those symptoms had lasted. Participants’ answers to these questions have been combined with genetic data and have been used to gain a number of insights, including the identification of potential genetic factors underlying COVID-19 (these studies are still ongoing)1-4.
Even in mild cases, symptoms persist
In the course of carrying out various studies using participants’ survey data, researchers recognized a pattern in survey respondents’ symptoms: Among people who had at least one symptom of illness, people who tested positive tended to report experiencing more symptoms than those who tested negative; and, the more symptoms a person had, the longer they were likely to have them. This result was consistent with the findings from previous studies5,6 that were limited to people suffering from severe COVID-19—meaning they had to go to the hospital and in some cases receive mechanical respirators to help them breathe.
This gif highlights the finding that people with >5 initial symptoms are much more likely to experience long term symptoms by first showing the total number of individuals in each category (with less than 5 initial symptoms or equal to/more than 5) and then showing how many within those categories also had longterm symptoms.
Among survey respondents in this study, 233 reported testing positive for COVID-19, 3,692 reported having tested negative, and 17,474 said they had not been tested. Among those who tested positive, only 8 of them had been to the hospital.
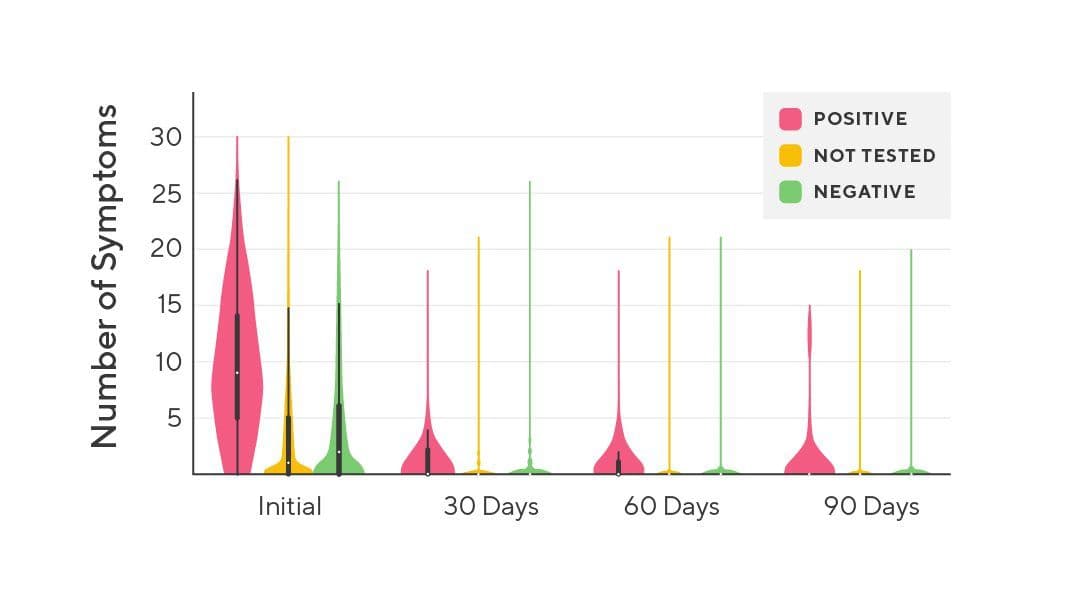
The above image is a violin plot. The height of each column shows the range of the data, and the width shows the distribution of data points along that range. This one in particular shows the number of symptoms reported in all individuals at each timepoint.
The team of researchers split the data up into groups, first organizing participants’ data based on their testing status and then again based on how many symptoms they initially report having (greater than 5 vs. 5 or fewer). In analyzing each group’s symptoms, researchers found that almost half (43.4%) of people with COVID-19 reported having symptoms that lasted longer than 30 days, and nearly a quarter (23.3%) had at least one symptom persist 90 days after testing positive. In contrast, only 9% of people without COVID-19 reported having symptoms that persisted for periods longer than 30 days.
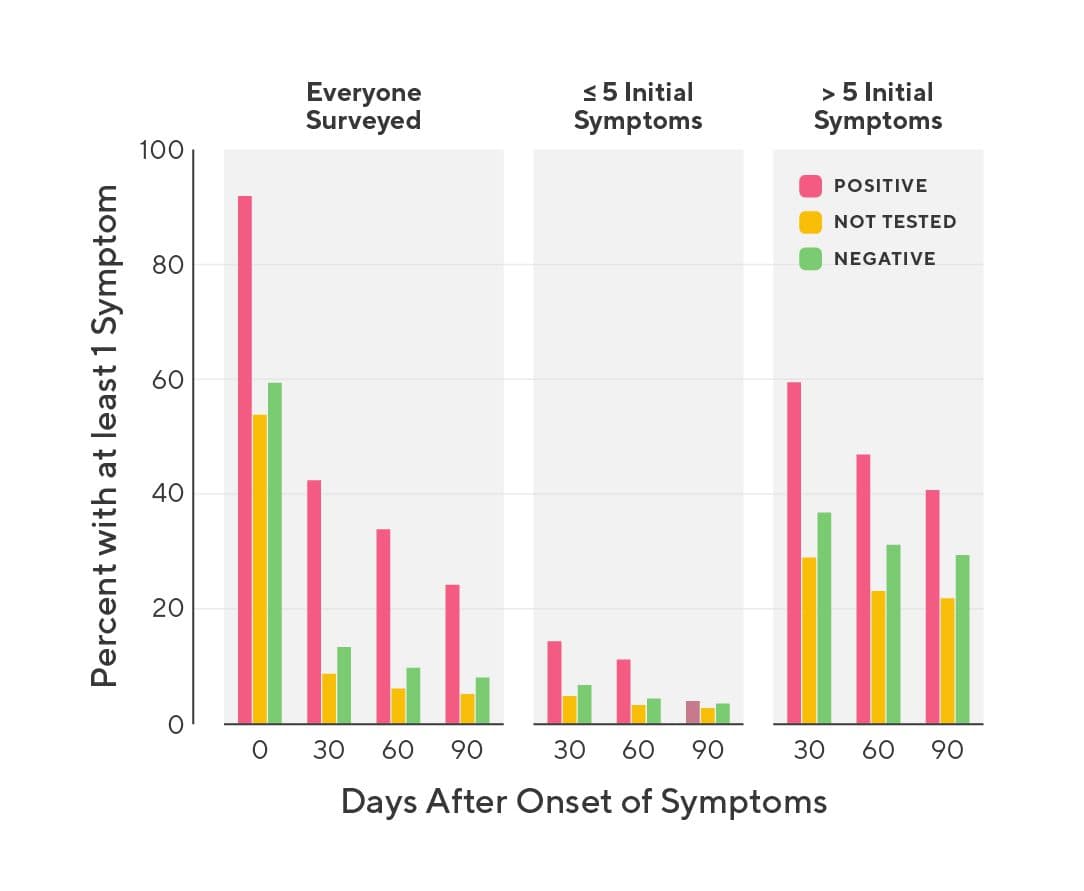
Percent of participants with at least one symptom during the study period (initial), or at least one symptom that lasted longer than 30 days, 60 days, or 90 days.
Symptoms without COVID-19?
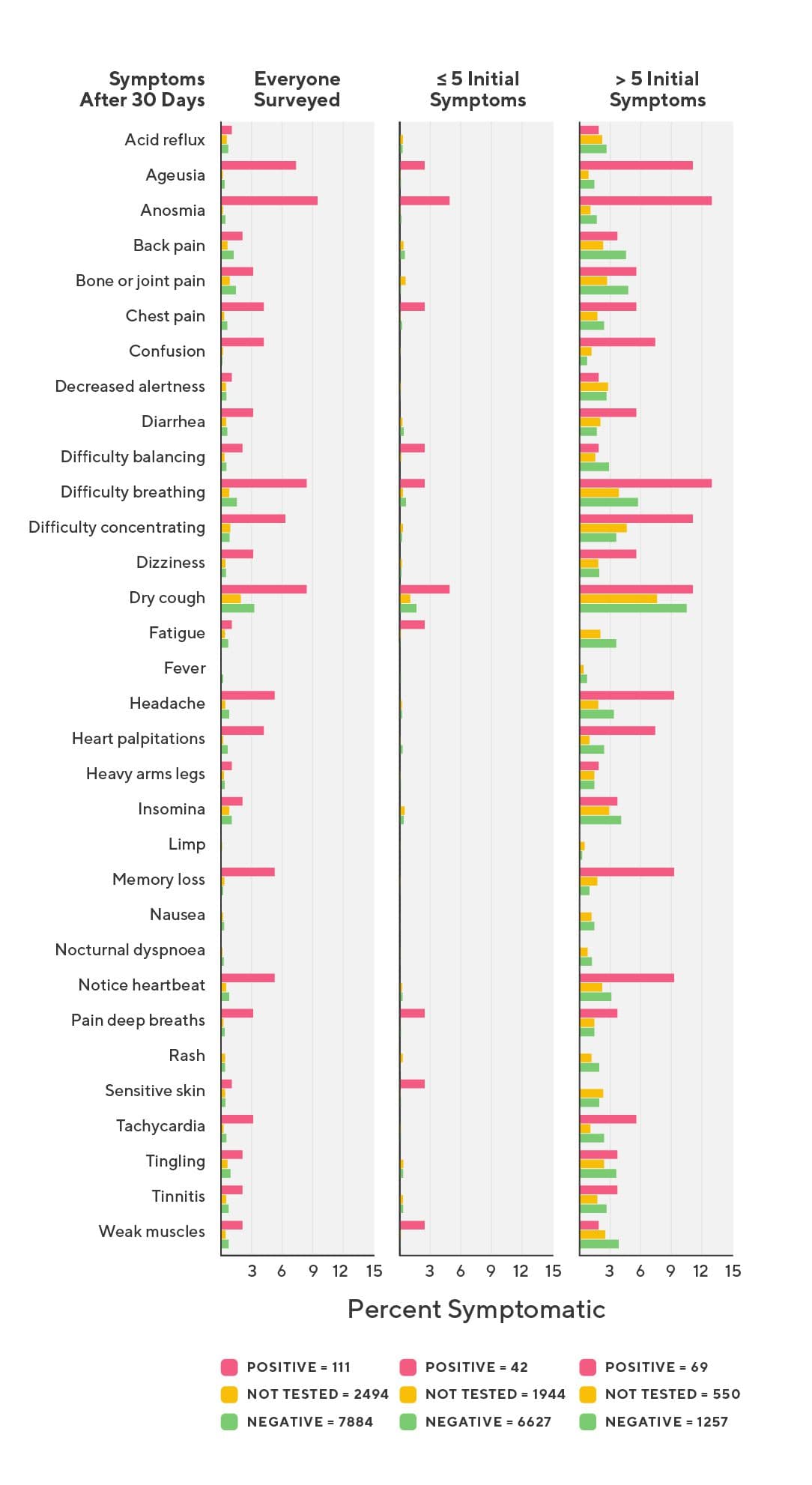
It is important to remember that symptoms of COVID-19 are not unique, and many of the symptoms associated with COVID-19—headache, chest pain, dry cough—are common and can stem from a number of different causes. However, there is a clear trend wherein people with COVID-19 report these (and other) symptoms more frequently than people without COVID-19. It is also possible that some people who tested negative (or weren’t tested) had been infected with SARS-CoV-2 but weren’t detected due to timing—if you test someone too early or too late after infection, they may not have detectable levels of virus in their system—or lack of specificity in the test used. Finally, many individuals in this study live in the western United States which has seen significant wildfires this year. Smoke from these fires may have increased the total frequency at which certain symptoms were seen.
The long-term symptoms that were significantly enriched in people with COVID-19 included partial loss of smell or taste, difficulty concentrating, difficulty breathing, memory loss, confusion, headache, heart palpitations, chest pain, pain with deep breaths, tachycardia, and dry cough.
It’s not clear how these genetic factors may influence a person’s vulnerability to COVID-19, but it may relate to how cells respond to viral infection. As with most findings in research, more research will be needed to make sense of this study’s findings.
It is noteworthy, too, that people who experienced more than 5 symptoms at the onset of illness, regardless of their test status, experienced longer bouts of illness. This trend was exacerbated in those with COVID-19, as roughly 40% of people who had more than 5 initial symptoms and tested positive for COVID-19 had continuing symptoms 90 days out.
Previous studies have reported that 74-88%5,6 of people who experience severe COVID-19 had symptoms that persisted longer than 60 days, and others have found lung abnormalities as much as 24 days post-infection7. Another study reported heart abnormalities in 78% of severe COVID-19 patients8. The data reported here is unique in that researchers included mild cases of COVID-19 in their assessment and still found evidence of persistent symptoms. Taken together, this body of evidence suggests that SARS-CoV-2 infection can have a lasting impact on people’s health, even among mild cases.
Why this is the case is still unknown and a topic that will continue to receive significant attention within the research community.
To read the full details from this study, a preprint has been posted on MedRxiv.
References
1. Zhang Q;Bastard P;Liu Z;Le Pen J;Moncada-Velez M;Chen J;Ogishi M;Sabli IKD;Hodeib S;Korol C;Rosain J;Bilguvar K;Ye J;Bolze A;Bigio B;Yang R;Arias AA;Zhou Q;Zhang Y;Onodi F;Korniotis S;Karpf L;Philippot Q;Chbihi M;Bonnet-Madin L;Dorgham K;Smith N;Schneider. “Inborn Errors of Type I IFN Immunity in Patients with Life-Threatening COVID-19.” Science (New York, N.Y.), U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/32972995/
2. Bastard, Paul, et al. “Auto-Antibodies against Type I IFNs in Patients with Life-Threatening COVID-19.” Science, American Association for the Advancement of Science, 24 Sept. 2020, science.sciencemag.org/content/early/2020/09/23/science.abd4585.full.
3. Ellinghaus, David, et al. “Genomewide Association Study of Severe Covid-19 with Respiratory Failure: NEJM.” New England Journal of Medicine, 8 Oct. 2020, www.nejm.org/doi/10.1056/NEJMoa2020283.
4. Blokland, Irene V van, et al. “Using Symptom-Based Case Predictions to Identify Host Genetic Factors That Contribute to COVID-19 Susceptibility.” MedRxiv, Cold Spring Harbor Laboratory Press, 1 Jan. 2020, www.medrxiv.org/content/10.1101/2020.08.21.20177246v1.
5. Arnold, David T, et al. “Patient Outcomes after Hospitalisation with COVID-19 and Implications for Follow-up; Results from a Prospective UK Cohort.” MedRxiv, Cold Spring Harbor Laboratory Press, 1 Jan. 2020, www.medrxiv.org/content/10.1101/2020.08.12.20173526v1.
6. Carfì, Angelo, et al. “Persistent Symptoms in Patients After Acute COVID-19.” Jama, vol. 324, no. 6, 2020, p. 603., doi:10.1001/jama.2020.12603.
7. Wang, Y. et al. Temporal Changes of CT Findings in 90 Patients with COVID-19 Pneumonia: A Longitudinal Study. Radiology 296, E55–E64 (2020).
8. Puntmann, V. O. et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol (2020) doi:10.1001/jamacardio.2020.3557.
Categories