Eczema often runs in families. This gene may explain why

Eczema is a non-contagious, long-lasting, inflammatory skin condition that often results in patches of skin becoming dry and itchy. For sufferers, the urge to scratch the itch can be overwhelming, but doing so can just make the urge worse. Fortunately, there are ways to lessen the itch without scratching, and it all starts with an understanding of what eczema is, and what causes it.
Before we get into it, we should clarify some terminology. “Eczema” is a term that commonly describes a condition known as atopic dermatitis. Though “eczema” is now synonymous with “atopic dermatitis,” its original meaning specifically described a common symptom of many skin conditions—dry, itchy skin lesions—and not any one condition in particular. In this article, we use the more common meaning of “eczema” as a stand-in for “atopic dermatitis.”1
Now, let’s go beyond the surface and look at what causes eczema and, more importantly, what can be done about it. The characteristic patches of irritated, dry, and itchy skin tend to come and go, and can vary significantly in severity, size, and in how often they appear2,3. These symptoms are primarily a result of a triggered immune system that’s perceived a potential threat to the body—specifically in the part of the skin that’s developing into an itchy lesion—and has responded by increasing inflammation in the affected area2. But why would the immune system think there’s a problem? The answer involves a combination of our environment, our DNA, and our skin.
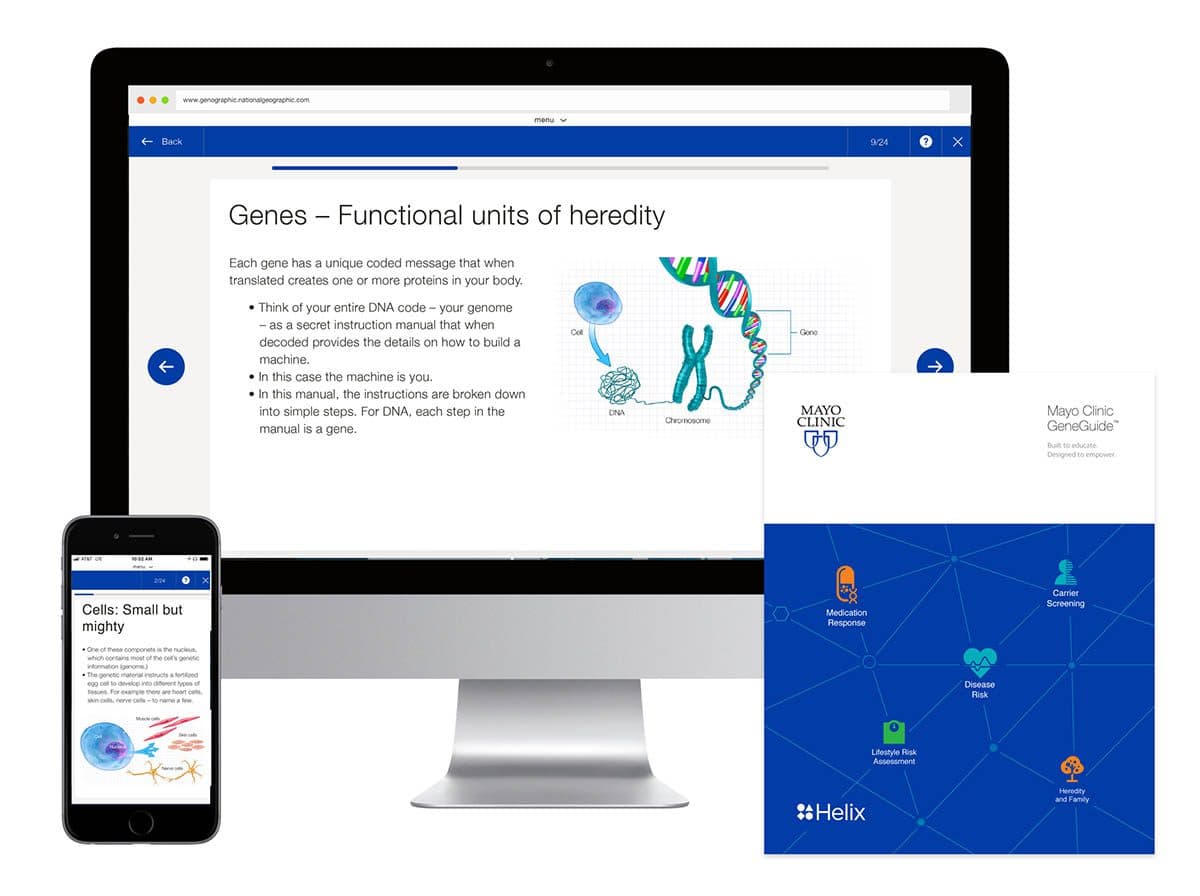
Mayo Clinic GeneGuide™ is a genetic testing experience that helps you understand how genetics can affect your health.
Scientists have known for a long time that eczema is heritable, but it wasn’t until 2006 that they first identified a gene that may be responsible for this condition4. The gene is known as FLG and it is a particularly large segment of DNA that codes for a protein called profilaggrin. The size of the gene is actually so large, and the sequence so complex, that it was one of the last genes in the human genome to be fully sequenced4. But it’s good that it was sequenced, because researchers have found that changes to the DNA sequence in this gene can predispose a person to eczema.
Profilaggrin is made by cells in our skin and it serves an important role in sealing us off from the outside environment. How it does this is a complex process, but in essence profilaggrin is broken down into medium-sized chunks of protein that help bind important structures to one another in our skin to form a solid barrier. Those chunks can be broken down further into small pieces of protein that form a liquid-like meshwork that helps to further build out our skin barrier. As a whole, this barrier helps protect us from damaging UV light, prevents excessive water loss, and keeps potentially harmful objects from slipping past our skin and entering the body4,5.
Fortunately, Mayo Clinic GeneGuide may be able to help
As it happens, many people—possibly as many as 10% of people in some populations—inherit at least one version of the FLG gene that has a slightly different DNA sequence2. These changes in the DNA sequence have been shown to decrease the amount of profilaggrin protein that gets made2,4. As a result, the skin barrier is less able to prevent both water loss and the entry of pathogens. Our skin is constantly keeping track of our environment’s humidity and, when the humidity drops, skin cells will start to produce more of the profilaggrin protein to prevent water loss. With eczema, this means that a person’s skin is prone to drying out—and irritants like pollen, mold, and some food allergens can slip past the skin barrier and cause the immune system to activate, ultimately resulting in inflammation and itchiness5.
Itching isn’t unique to eczema, so the condition is often overlooked. Researchers have observed that people who inherit just one version of an eczema-associated FLG gene may have less severe symptoms, meaning many people are unaware of the underlying cause of their itch2,3. Fortunately, Mayo Clinic GeneGuide may be able to help.
Mayo Clinic GeneGuide helps people learn about their DNA and some of the many ways it may be impacting their lives, including an analysis of the FLG gene. Finding out if you’re genetically predisposed to eczema may help you stay vigilant for the signs of eczema, and talk to your health care provider if you’d like to learn about treatment for it.
Thus far, researchers have not come to a conclusion about whether eczema ever truly resolves itself. However, treatments are available to help lessen its impact. The NIH recommends a series of at-home skin care tips that include avoidance of scratching, frequent moisturizing with non-alcoholic moisturizers, and use of a humidifier to maintain a humid environment.
It’s important to note that many people who are predisposed to eczema never develop the condition2,3. This points to the fact that DNA is not destiny, and our environment can influence whether or not we develop conditions like this. To learn more about eczema and how your DNA intersects with health, consider starting your journey with Mayo Clinic GeneGuide.
- Xu, Shuai, et al. “Eczema, Atopic Dermatitis, or Atopic Eczema.” Dermatitis, vol. 28, no. 4, 2017, pp. 276–279., doi:10.1097/der.0000000000000273.
- “Overview of Atopic Dermatitis.” AJMC, www.ajmc.com/journals/supplement/2017/atopic-dermatitis-focusing-on-the-patient-care-strategy-in-the-managed-care-setting/overview-of-atopic-dermatitis-article.
- Abuabara, Katrina et al. “The Long-Term Course of Atopic Dermatitis” Dermatologic clinics vol. 35,3 (2017): 291-297.
- McLean, W H I. “Filaggrin failure – from ichthyosis vulgaris to atopic eczema and beyond” British journal of dermatology vol. 175 Suppl 2,Suppl Suppl 2 (2016): 4-7.
- Sandilands, Aileen et al. “Filaggrin in the frontline: role in skin barrier function and disease” Journal of cell science vol. 122,Pt 9 (2009): 1285-94.
Categories