5 ways Helix’s research community has advanced science in 2020
As we wrap up 2020 and look back at the year we’ve all endured, it’s important to highlight the places where humanity shone through the darkness. One such place is in our research community.
While the people around the nation were forced into isolation by stay at home orders or self-imposed quarantine, our research community rallied together (virtually) to help advance our understanding of science, and particularly to help us fight back against COVID-19.
Thousands of people from the Helix research community have volunteered their time to fill out our ongoing COVID-19 survey. In the moment, this can feel like a small act, but the impact has been immense.
Over the past year, Helix’s research community has contributed to numerous advances in science, some related to COVID-19 and others related to genetics more broadly.
Here, we’ll take a quick look back at all that we’ve accomplished together. In what has been a tough year for many, we hope you can feel some pride in having taken part in such groundbreaking work! As always, we thank you for your continued support and dedication to bettering our world.
1. DNA may influence a person’s vulnerability to severe COVID-19
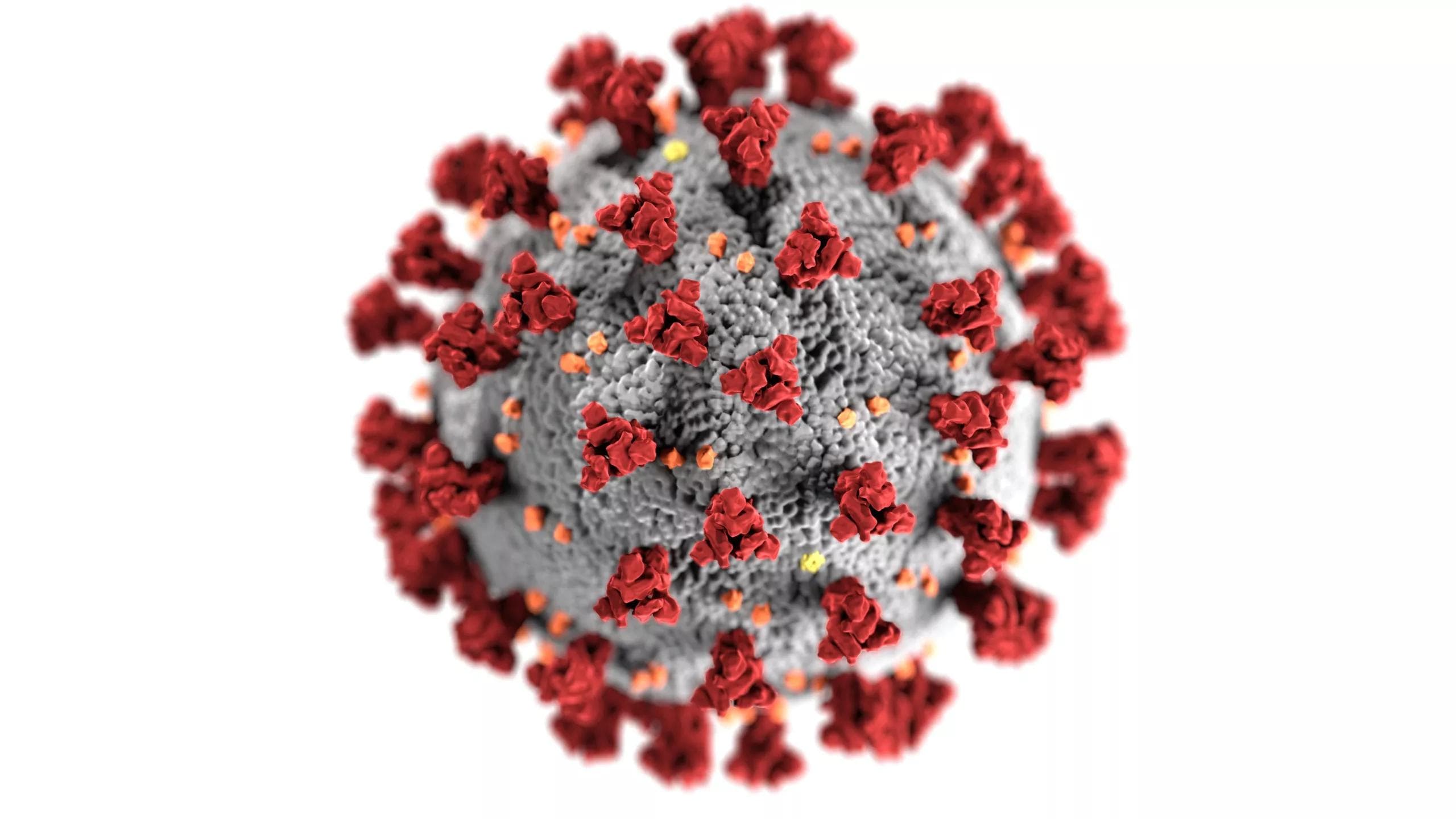
Early in the pandemic, it became clear that we were dealing with a complex disease. COVID-19 caused lethal symptoms in some people, while other people showed no symptoms at all. What’s more, some people who would have surely come into contact with the SARS-CoV-2 virus—the one responsible for COVID-19—seemed to remain uninfected.
Why the difference? Why aren’t all people equally affected?
Time has shown us that there are many factors at play here, such as your environment, pre-existing conditions, and, possibly, your DNA.
DNA has proven to affect people’s vulnerability to viruses in the past. One notable example of this can be found in the AIDS pandemic. Researchers found that a small group of people who carried a specific factor in their DNA were less likely to be infected with HIV. This factor altered the way their body made a protein that sits on the surface of it’s cells. As it happens, that protein is vitally important for the HIV virus to enter cells and infect a person. The alteration brought on by the genetic factor these people carried protected them from the virus.
As the COVID-19 pandemic blazed around the world, researchers began to wonder if the same thing might be true for the SARS-CoV-2 virus: Could there be genetic factors that decrease (or increase) a person’s chances of being infected? Similarly, could there be genetic factors that affect how severe a person’s symptoms are once they’re infected?
Helix’s research community—comprising tens of thousands of people—went to work answering these questions in collaboration with an international network of scientists.
A survey was sent out to this community asking them about their exposure to COVID-19, whether they had been tested, what symptoms they may have been experiencing, and related information. These data were then paired with each respondent’s genetic data and used by researchers who were looking for patterns, patterns that would suggest an association between genetic factors and vulnerability to severe COVID-19.
These data have led to numerous publications, two of which have made a splash in the research community1-5. The first was generated with a team of researchers from around the world who collaborated with Helix scientists. Together, the team found that people who developed severe symptoms of COVID-19 tended to have variations in their DNA sequence that occurred in the same part of the DNA. It’s not clear yet how changes to the DNA sequence in this location could affect a person’s response to COVID-19 infection, but it may have to do with immune cells—one of the genes located in this part of the DNA have previously been shown to play a role in helping immune cells operate in the lungs.
This finding has since been replicated in numerous studies, suggesting that something about this part of DNA is important.
The next big finding came in September. Here, another collaboration with researchers from around the world revealed that alterations in the DNA that affect the body’s innate immune response could be responsible for as much as 3.5% of severe COVID-19 cases3. Put another way, it appears that changes to the DNA that decrease the body’s ability to mount a rapid response to the virus seem to have caused many people to develop severe symptoms. Had their body been able to respond to the virus quickly, they might have only developed mild symptoms (if any at all).
This finding was huge because it was the first time scientists had been able to identify a location in the DNA that is not only associated with severe COVID-19, but they had evidence to show that it was likely causing severe COVID-193,4. And, Helix data helped them in this research.
Helix’s survey data has contributed to multiple publications in 20201-5, each of which has helped us better understand the relationship between DNA and COVID-19. To be sure, it is a complicated relationship and one that we don’t yet understand. But these small victories are moving us forward in big ways, and that is due in part to Helix’s research community.
2. The important and enduring nature of COVID-19 symptoms
One of the major issues in responding to the COVID-19 pandemic has been a lack of available testing. The gold standard for COVID-19 testing is the use of a PCR test which detects the presence of viral genetic material. However, this type of testing was hard to come by in the early days of the pandemic, and is still difficult to find in some places today.
Without access to PCR testing, some researchers have relied on identifying people who likely have, or had, COVID-19 based on their symptoms2. This is a difficult task, though, because the list of symptoms associated with COVID-19 is both long and not very unique—many of the symptoms overlap with other conditions, such as the common cold.
Helix’s COVID-19 survey offered a way for researchers to study the symptoms of COVID-19 and narrow in on what is truly characteristic of this disease5.
In a recent paper that Helix published as a pre-print (meaning it has yet to go through peer review), Helix scientists outlined symptoms of COVID-19 and their enduring nature. Among the findings were two big insights: That researchers need to consider the number of initial symptoms when studying COVID-19 symptoms, and that even in mild cases of the disease, symptoms can last for a very long time.
The former insight is important because if we want to narrow in on symptoms that doctors and others can use to quickly identify COVID-19, we need to be able to separate these symptoms from other causes. Helix’s team found that, when trying to identify symptoms that strongly predict COVID-19, it is important to compare cases and controls (people who report symptoms and say they tested positive vs. people who report symptoms but say they tested negative) who have a similar number of symptoms. In doing this, you can be more accurate in narrowing in on characteristic symptoms.
The enduring nature of COVID-19 symptoms was surprising. Much of the media coverage around COVID-19 has centered on severe cases. But here, it was shown that even in mild cases, some people experienced symptoms for more than 90 days. This is supported by reports from other teams, and sheds light on the long-term impact of this widespread disease.
3. New connections between rare genetic changes and our traits
The insights generated by Helix’s research team weren’t limited to COVID-19. In January of this year, the team published a paper reporting the discovery of new connections between our DNA and our traits that were found using a relatively new approach6.
Rare variants are changes in a person’s DNA that are very rarely seen in others. We all have them, and most of the time they have no effect on us. What the Helix team did was analyze DNA sequences from 70,000 people with a specific focus on rare variants. They then looked for hot spots – where there are rare variants occurring in close proximity to one another specifically in people who have certain diseases or traits.
With this analysis, they found several new associations and highlighted for the research community that collapsing rare variants together into these hot spots can be a powerful way to make new discoveries.
4. An influence of genetics in type 2 diabetes
Diabetes is often thought of as a cut-and-dry condition where a person either has type 1 diabetes, type 2 diabetes, or what’s known as monogenic diabetes (conditions caused by particularly impactful genetic factors).
However, evidence suggests that these neat categories might be more complex than we thought.
Helix’s research team took part in a collaborative project exploring the impact of genetics on type 2 diabetes7. They found that some individuals who are diagnosed with type 2 diabetes tend to carry variants in a specific part of the DNA. These variants appear to cause high blood sugar levels, though these people tend to be otherwise healthy. And, importantly, they seem less responsive to normal medications prescribed to people with type 2 diabetes.
This finding is significant because it suggests that people who have these genetic factors may benefit from different therapeutic strategies (in some cases, they may not have to take medication at all). There will need to be many follow up studies to confirm this, but the results are truly exciting and will inspire much more research.
5. The benefits of population genetic screening
DNA sequencing has long been out of reach for most people. The cost has historically been high, and unless you had symptoms of disease, the benefits of being sequenced were fuzzy.
Advances in our understanding of genetics have changed this. Sequencing costs much less now, and the information we can gain from a person’s DNA may help improve their healthcare and could even save their life by helping doctors to identify underlying genetic disease. However, there remains a big hurdle: is it practical and beneficial to offer DNA sequencing en masse?
Helix scientists published a paper in collaboration with the Healthy Nevada Project suggesting that broad-scale genetic testing is not only practical, but hugely beneficial8.
Through the Healthy Nevada Project, more than 20,000 people from Northern Nevada were sequenced. Participants received a free genetic ancestry report and were screened for three highly actionable conditions (Familial Hypercholesterolemia, hereditary breast and ovarian cancer, and Lynch Syndrome.) Each of these conditions can be detected using DNA sequencing technology and each of them are thought to be largely under-diagnosed because so few people undergo DNA sequencing.
If found to have one of these conditions, participants can work with their doctors to take preventative measures that will help to mitigate the impact of the disease, and possibly even prevent the disease from developing.
Helix’s team found that as many as 1:75 people had one of these conditions, and 90% of them would not have been diagnosed had they not participated in the Healthy Nevada Project8. This is a huge finding because it suggests that there is a large public health benefit in offering broadscale genetic screening.
A year to be proud of
This year has been hard for all, but there have been some notable victories along the way. We are very proud of our research team and the broader research community. By rallying together and working to make these discoveries, we truly are helping to improve public health and are making the world a better place.
Thank you to all of you who have participated and to all who will participate in the years to come. We look forward to continuing to work on research projects that advance genomic medicine in 2021 and beyond.
References
1. Group*, The Severe Covid-19 GWAS, et al. “Genomewide Association Study of Severe Covid-19 with Respiratory Failure: NEJM.” New England Journal of Medicine, 15 Oct. 2020, www.nejm.org/doi/full/10.1056/NEJMoa2020283.
2. Blokland, Irene V van, et al. “Using Symptom-Based Case Predictions to Identify Host Genetic Factors That Contribute to COVID-19 Susceptibility.” MedRxiv, Cold Spring Harbor Laboratory Press, 1 Jan. 2020, www.medrxiv.org/content/10.1101/2020.08.21.20177246v1.
3. Zhang, Qian, et al. “Inborn Errors of Type I IFN Immunity in Patients with Life-Threatening COVID-19.” Science, vol. 370, no. 6515, 2020, doi:10.1126/science.abd4570.
4. Bastard, Paul, et al. “Autoantibodies against Type I IFNs in Patients with Life-Threatening COVID-19.” Science, American Association for the Advancement of Science, 23 Oct. 2020, science.sciencemag.org/content/370/6515/eabd4585/tab-pdf.
5. Cirulli, Elizabeth T., et al. “Long-Term COVID-19 Symptoms in a Large Unselected Population.” MedRxiv, Cold Spring Harbor Laboratory Press, 1 Jan. 2020, www.medrxiv.org/content/10.1101/2020.10.07.20208702v3.
6. Cirulli, Elizabeth T., et al. “Genome-Wide Rare Variant Analysis for Thousands of Phenotypes in over 70,000 Exomes from Two Cohorts.” Nature News, Nature Publishing Group, 28 Jan. 2020, www.nature.com/articles/s41467-020-14288-y.
7. Bonnefond, Amélie, et al. “Pathogenic Variants in Actionable MODY Genes Are Associated with Type 2 Diabetes.” Nature News, Nature Publishing Group, 12 Oct. 2020, www.nature.com/articles/s42255-020-00294-3.
8. Grzymski, J. J., et al. “Population Genetic Screening Efficiently Identifies Carriers of Autosomal Dominant Diseases.” Nature News, Nature Publishing Group, 27 July 2020, www.nature.com/articles/s41591-020-0982-5.
Categories